In fight against opioid abuse, law enforcement takes aim at physicians
Published 12:52 pm Thursday, April 14, 2016
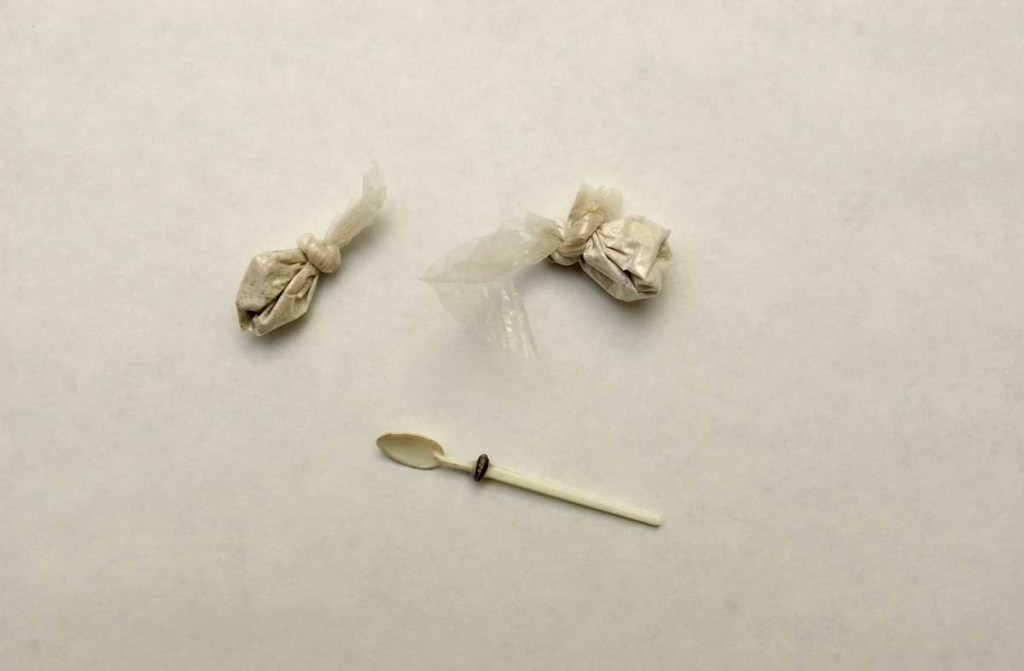
- Two twists of heroin and a small spoon used to scoop the drug.
Many experts agree that America is in the grip of a full-blown heroin epidemic, and law enforcement officials are increasingly holding doctors accountable for questionable prescribing practices that some say can lead to a dependence on heroin.
“There’s absolutely no doubt that the overprescribing and over-availability of these opioids is a direct link to the spike in heroin use,” says Indiana Attorney General Greg Zoeller.
According to the Centers for Disease Control and Prevention, the rate of overdose deaths involving opioids, both heroin and prescription drugs, has nearly quadrupled since 1999; and approximately 78 Americans die each day from an opioid overdose.
Several recent cases in Pennsylvania, Indiana and elsewhere — some of which have included allegations of drugs exchanged for sex — have seen doctors lose their licenses and receive prison sentences for prescribing oxycodone and other narcotic painkillers in dangerously high volumes. Increasing action against physicians is a trend that some see as necessary in order to curb heroin usage, which often results from patients seeking to avoid withdrawal symptoms when their prescriptions run out. A 2014 CDC study found that nearly three out of every four people who overdosed on heroin or other opioids started with a prescription for painkillers.
In Indiana, Zoeller launched a statewide task force in 2012 to address the problem of rising prescription drug abuse. Drug overdoses were blamed in more than 1,000 deaths in the state that year, an increase of 57 percent over the last decade.
“It’s taken years and years of overuse before there was finally some administrative regulation taken,” said Rodney Cummings, a prosecutor in Madison County, Indiana, where police raids have taken nearly 50 dealers and users off the streets in the last two years. “There was a problem here, and I think there was a strong reaction from the federal government to take a much more aggressive approach.”
The county’s community health center is at the center of an ongoing federal lawsuit alleging that the facility profited by prescribing unnecessary narcotics to most of its patients. The center’s medical director, Dr. Frank Campbell, surrendered his license to prescribe controlled substances in 2013 after it was found he had allowed two of his assistants to use prescription pads he had pre-signed, sometimes days before patient appointments. Under law, such prescriptions are to be signed only on the day of an exam.
Zoeller points to that case as an example of the government’s strategy to curb heroin usage by choking off potential supply points. Last year, his office took action against more than 130 license holders — including doctors, pharmacists, nurses and dentists — for alleged violations of prescription drug diversion and overprescription.
“As we’ve cut into the vast oversupply, there’s probably fewer people entering the cycle of addiction,” he said. “We have to do this. We have to get back to proper prescribing only where it’s absolutely necessary and not as a first course of action.”
The CDC has recently updated its guidelines for prescribing opioids and other pain relieving drugs, reflecting concern about the risks and benefits of opioid therapy for chronic pain.
Many medical professionals, while agreeing that more aggressive police action against those physicians who overprescribe could help stem the tide, caution against moving too quickly.
“We have to find a way to address the issue that does everything we can to eliminate these opiates while not harming those patients who are being followed appropriately by a well-trained medical professional for a problem that is well established,” says Dr. Scott Shapiro, a cardiologist in Abington, Pennsylvania who serves as president of the Pennsylvania Medical Society. “That’s a difficult balance, but one that physicians are tackling head-on.”
Shapiro notes that his organization is working with the state’s department of health to create more rigorous prescription guidelines and will continue to support law enforcement efforts to root out criminal activity in the medical profession. But he also urges awareness of the “unintended consequences” of potential harm to patients who have appropriate prescriptions.
“You can’t arrest your way out of these problems,” he said. “You can’t throw out all of these narcotics and not allow anyone to prescribe them. There shouldn’t be a stigma attached to someone who is under the care of a well-qualified physician.”





