Internet delivers one-on-one healthcare to rural Georgia
Published 4:30 pm Friday, October 16, 2015
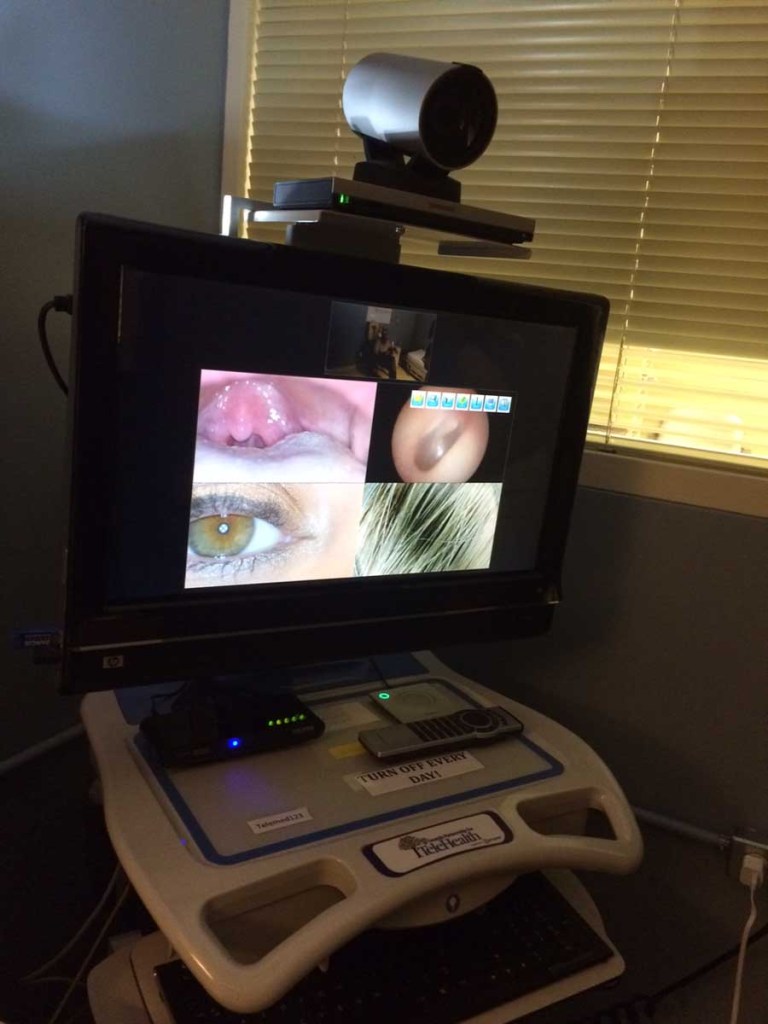
- A screen shows images taken during a recent session with a student, who was complaining of a sore throat. Last year, Tift Regional's doctors saw 150 students in school-based health clinics, with some as far away as Candler County near Statesboro, Georgia.
TIFTON, Ga. – During its first year, the telemedicine machine at Tift Regional Medical Center was nothing more than a glorified Internet portal.
The hospital staff wasn’t quite sure what to do with it. With few people connected, the world of telemedicine was a lonely place.
That was nearly a decade ago. Now, the hospital in south Georgia uses the technology to connect patients with specialists in cities including Atlanta, Macon and Augusta.
The sprawling healthcare network is both changing rural medicine and offering a glimpse of what some believe will be the future of healthcare everywhere.
Tift Regional was an original partner in a telemedicine network that now connects more than 600 hospitals, schools, jails, nursing homes and primary care clinics with more than 250 physicians.
Some specialists aren’t even in the state – or the country.
“This is the miracle of telemedicine; it erases time and distance,” said Jeff Robbins, director of telehealth at Tift Regional. “Why would you go to Atlanta if you don’t have to?”
The hospital also links its own physicians with school kids across Georgia. Last year, Tift Regional’s doctors saw 150 students in school-based health clinics, with some as far away as Candler County near Statesboro.
But, for the most part, the program creates access to services that otherwise aren’t available in the area.
Telemedicine, or telehealth, is really just a secure Skype connection, Robbins said. At Tift Regional, cameras are attached to computers and can be rolled to wherever they’re needed.
Add-ons really help bridge the distance. Doctors on the other end can hear a patient’s heartbeat through a Bluetooth-enabled stethoscope. An otoscope equipped with a camera provides a close-up view of the inner ear.
Tift Regional logged 1,100 of these virtual doctor-patient encounters last year for services ranging from pre- and post-op for kidney transplants to therapy with a pediatric psychiatrist.
“It’s not just a passing fad to us, it is the future,” Robbins said. “Actually, it’s not the future, it’s already here.”
The sentiment is not universally shared throughout Georgia.
“You can talk about this stuff all day long, but until people see it, they don’t get it,” said Paula Guy, who heads the Georgia Partnership for TeleHealth, a nonprofit that manages the state’s system.
“Doctors think you’re taking away from the patients. They think it’s too costly. They think, ‘Oh, it’s just a phone call,'” she said.
Increased awareness of the technology, she said, will convince people that it’s “real medicine.”
“If you’re not doing telemedicine today, you’re going to be doing it in the next few years. The public’s going to demand it,” she said. “It won’t even be called telemedicine in five years, I don’t think. It’s just going to be ‘healthcare.’”
More success stories, like what’s happening in Hancock County, will help the cause. The rural county, which no longer has a hospital, equipped ambulances so that EMTs in a patient’s home can connect with emergency-room doctors elsewhere.
Long-distance healthcare connections face other hurdles, as well. While regular telemedicine is covered, Medicaid and Medicare do not currently reimburse providers for remote patient monitoring, Guy said. Hancock County received a waiver for its program.
A state-funded pilot project is expected to sway more hospitals and communities to support telemedicine, although Guy said the real impact may not be apparent for a couple of years.
Lawmakers added $3 million to this year’s budget to launch hub-and-spoke programs that connect rural communities.
Four hospitals – Union General, Appling Health System, Crisp Regional and Emanuel Regional Medical Center – will serve as hubs. Spokes may include school clinics, public heath departments and ambulances equipped with WiFi and telemedicine capabilities.
“We are anticipating more growth and for the whole field to evolve more and help us, especially in rural Georgia,” said Sen. Greg Kirk, R-Americus, who represents Tift County and serves on the Senate’s Health and Human Services Committee.
In Tifton, the program started small.
Initially, the hospital only offered autism and other behavioral health services, connecting patients with a doctor in Atlanta.
Demand for pediatric services fueled the program’s growth. Tifton patients can now access pediatric gastrointestinal physicians and endocrinologists in Macon. Pediatric HIV and infectious disease specialists in Augusta will soon join the network.
The hospital also has an arrangement with Emory Healthcare’s kidney transplant program. Pre- and post-operation tests are often handled locally, while an Emory doctor performs the procedures and checks in with patients through video sessions.
Such arrangements keep patients – and money – in Tifton at a time when an alarming number of rural hospitals are reducing services or closing completely, Robbins said.
The Emory partnership brings in more than $600,000 every year because of what Robbins called ancillary services such as echocardiograms, MRIs and blood work.
Without that, the hospital only earns $22.50 for every patient it presents to doctors elsewhere, Robbins said.
Telemedicine also generates about $158,000 from behavioral health patients, $11,000 from school-based clinics and $2.2 million from stroke patients, according to a report from Tift Regional.
That stroke service, which is through an Augusta-based stroke program called REACH, connects the emergency room to an on-call neurologist.
“If you have a stroke out in a rural area, you’re up the creek without a paddle if you don’t have access to a neurologist, which most rural hospitals don’t have,” Guy said.
Robbins said the revenue that telemedicine represents for Tift Regional isn’t the real return on investment. The reward, he said, is watching someone who has had a stroke walk out of the hospital on his own.
“Everybody deserves a chance to be well,” he said. “Sometimes that means you have to get to a doctor, and not everyone can get to that doctor. Because of simple technology like this, it allows us to get the patient there.”
This isn’t to everyone’s advantage, though.
A local student complaining of a sore throat – often a ticket home from school – recently saw a Tift Regional doctor through a video conference.
An exam revealed no redness in the child’s throat or other signs of illness.
“The kid had to get back to class,” Robbins said.
Jill Nolin covers the Georgia Statehouse for CNHI’s newspapers and websites. Reach her at jnolin@cnhi.com.





